Deep Brain Stimulation in treating early Alzheimer's
How effective would DBS be in treating AD? Could it delay the prognosis and/or enhance quality of life? Many possibilities and lots of questions...
www.ncbi.nlm.nih.gov/pmc/articles/PMC3552463/pdf/icns_9_11-12_10.pdf (for the pdf article)
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3552463/ (for the link only)

The cause of AD has, in my mind, always been linked to the aggregation of amyloid plaques. However, I was unaware of the synergistic affects of the plaques coupled with a breakdown in communication between interconnected components of the brain. Before I could truly assess the feasibility of DBS I took some time to understand the mechanisms by which neural death occurs in AD. The reading mentioned something about the “default mode network,” a phrase I had never heard of before. According to Mevel et al, the default mode network (DMN) has been highlighted in neuroimaging studies as a set of brain regions showing increased activity in task-free state compared to cognitively demanding task, and synchronized activity at rest.1 Though, in this article, DMN changes are associated with AD changes within these areas, neural changes have been observed in healthy, aging individuals as well. The difference lies in the effect on several integrated pathways. In AD patients the functional connectivity between the PCC and the hippocampus [along with other components of the DMN] seems to be impaired.1As the disease spreads connectivity disturbances progress. With an understanding of the role defective DMN plays in progressive AD it became clear that focusing not only the removal of amyloid plaques but on the neurological connectivity within this specific region of the brain may be key in treating AD.
ReplyDeleteDr. DS, you weren’t kidding when you said “many possibilities and lots of questions”. Obviously DBS has shown promising results regarding the treatment of AD. However, the success of this procedure is contingent on the severity of AD at the onset of treatment. As interconnected portions of the DMN continue to decrease, chances of DBS being successful diminish as well. Being able to begin DBS at the onset of AD is imperative. However, it may become challenging to distinguish between the normal aging process and the forgetfulness associated with it and the cognitive impairments associated with AD.
I couldn’t help but question the success rate of this treatment and at what point in the progression of the disease will it dubbed useless? The article also emphasized the success of DBS in patients with early AD. I would be interested in knowing exactly what “early” is, in this case. It would also be interesting to observe the effectiveness of DBS on different connective components of the DMN. This paper emphasized the success of DBS in the hippocampal fornix region. What about the other components of the DMN? Will DBS be just as, if not more successful?
Though there are still many, many questions that I believe need to be answered before DBS can be dubbed the epitome of AD alternative medicine, I will say that if it were my mom or dad, grandma or grandpa who was suffering with AD I wouldn’t be opposed to exploring this unconventional option.
Resources
1. Mevel K, Chetelat G, Eustache F, Desgranges B. The Default Mode Network in Healthy Aging and Alzheimer's Disease. Int J Alzheimers Dis. 2011; 2011: 535816.
A close friend of mine who has Parkinson's (& has suffered from it for probably 20+ years) went in for DBS. Even though it has been remarkable for so many other sufferers, he had complications almost immediately, suffering a massive stroke that nearly killed him. He has since gone through years of physical therapy, rehabilitation, and even a stint in a nursing home; however, he still is not 100%. I think many people don't realize that even with procedures that are standard practices there can be unexpectated results. This isn't to dissuade anyone from undergoing these procedures, but they should be cognizant of all possibilities.
DeleteJess,
ReplyDeleteI agree with your statements. thank you for clearing up what default mode was.I'm curious as to if the default mode was much different for those with Alzheimer's as compared to someone that has normal elderly forgetfulness.
I agree with you in that it could be difficult to know when then disease actually started. How could we be certain that the treatment will work if we are not even certain at what point in progression the diseased person is actually in. I'm not sure myself if I would be okay with my parents testing a new treatment. My grandad has Alzheimer's. He is 96 and with careful watching he is doing well. I feel as though in his case that the treatment is too risky and he is quite old. It is doubtful for him that an Alzheimer's treatment will how long his life greatly. On the other hand, if my parents were to go in their fifties develop the disease, I might be willing to do whatever it took to prolong their lives. One of my fears though is that a treatment may cause the disease to accelerate as opposed to helping prevent it.
When I was reading the article, I got some different thoughts from it. I was wondering more about deep brain stimulation. Does one have to be in control of the electrodes? If so, how would it be known when to stimulate them? I found in a book about Parkinson's disease, that DBS comes with a stimulator that is placed in the chest cavity. It is pre-set to a degree of control (1). The book and article then state that there is a battery life of 3-5 years. That presents me with another question. How does one know when the battery dies? What if the battery is not changed in a quick manner? Would that cause an even quicker degredation? The brain had been used to being stimulated and it all of a sudden stopped instead of slowly stopping.
Another question I had was what would happen if there were trauma to any piece of the stimulator? Could there be great effects? Could a damaged stimulator cause very life threatening brain mistimulations?
Finally I wonder what the author meant by active on vs sham treatment in AD patients. Would there really be a group of patients left untreated? Is that ethical?
References:
1. National Collaborating Centre for Chronic Conditions (UK). Parkinson's Disease: National Clinical Guideline for Diagnosis and Management in Primary and Secondary Care. London: Royal College of Physicians (UK); 2006. (NICE Clinical Guidelines, No. 35.) 8, Surgery for Parkinson’s disease. Available from: http://www.ncbi.nlm.nih.gov/books/NBK48525/
The battery/controller is akin to a pacemaker and is magnetically controlled. When the battery begins to decline, the unit has to be replaced. I used to have something similar (that I used to rhetorically call my spinal pacemaker since the controller/pump was in my abdominal wall with a port that led to my spine), but it failed after a couple of years. Then I developed an infection surrounding the unit that spread through my lymph nodes. I had to go and have it all removed.
DeleteMedicine has become so advanced that we can now prevent many diseases and problems that once were deadly, allowing us to live longer. While this is amazing, it has opened us up to many complications with aging, one being degenerative diseases like Alzheimer’s. The unpredictable nature of Alzheimer’s and the fact that it is seemingly unstoppable make it a primary subject in research. Some drugs, like donepezil hydrochloride1, have been developed to slow down the progression of Alzheimer’s, but, so far, nothing has been able to stop it. This has only increased the need for more research into what causes Alzheimer’s and how it can be stopped.
ReplyDeleteA few years ago, my grandma was diagnosed with Alzheimer’s. She currently takes donepezil hydrochloride, but her memory is still deteriorating. Of course it is difficult to tell if the medication is helping or not, since the only way to know would be to take her off it and see if she deteriorates any faster. I would love to see a better treatment or a cure come before it’s too late for her.
Studies into DBS look very interesting, especially since, according to the article, DBS has been used to treat other brain diseases successfully. In 2010, a lady with severe depression was successfully freed of symptoms by DBS. However, I think it is important to note that DBS was used as a last resort2. The article says the lady “could not be helped by medication or electroconvulsive therapy”2. I can understand that people have tried everything else may look to DBS, and I think studies into its effectiveness should be continued.
However, many of the diseases described in the article as being treatable by DBS are diseases that do not cause death or do not cause it as quickly as Alzheimer’s does. In those cases, DBS can greatly improve people’s quality of life. In Alzheimer’s, unless DBS can stop the progression of the disease, it doesn’t seem worth it. The risks associated with DBS seem to great, if DBS only slows down the progression of Alzheimer’s. There are medications that slow down Alzheimer’s, and they come with much less risk than DBS.
Especially since many of the people that develop Alzheimer’s are elderly, the risks associated with DBS should be taken into account. If I were looking into DBS as a possible treatment for my grandmother, I would have many questions. How likely is she to have an adverse reaction to DBS? How likely is DBS going to work? To what extent is it expected to slow down or improve her memory? How risky is the procedure itself for an elderly woman? Is it worth it to go through all of this, or is it better for her to just continue taking donepezil hydrochloride? How effective, if at all, would DBS be in restoring memory loss?
The article ended by stating that DBS may be a potential treatment along with medications or treatments that slow down or stop plaque buildup. Since Alzheimer’s is mainly believed to be caused by chemical imbalances in the brain and a buildup of plaque causing cell death3, I agree that more research should be continued in both of these areas.
1. http://alzheimers.emedtv.com/aricept/aricept.html
2. http://www.sciencedaily.com/releases/2010/01/100108101435.htm
3. http://www.medicalnewstoday.com/articles/159442.php
This was a very informative journal article that focused in on Alzheimer’s disease (AD) and some of the key treatments in assisting in curing disease. The author of the article gave an in depth explanation of AD. Researchers of the article mainly focused on the specific treatment called deep brain stimulation (DBS).
ReplyDeletePersonally, I believe that this specific treatment would only be slightly effective. According to the author the research that supports this article seems to be uncertain and not very reliable. There are a few statements throughout the article that are not dependable. However, I do believe that this treatment would enhance the quality of life. AD is basically caused by the aggregation of amyloid plaques. As discussed in the article this treatment has been successful in early AD. My question for these researchers is how many successful studies have been performed in mid or late AD cases. Additionally, how successful are these DBS treatments done in humans because the articles mention that mice were the test subject. I would also like to know if this treatment is actually affordable. This treatment seems like it could be a very costly procedure. Even thought this treatment has a low risk rate I just feel like there is always a high risk when it comes to dealing with the brain. This disease involves the default mode network which is composed of many different sensitive and delicate portions of the brain. Honestly I just don’t trust this treatment but I do have a free mind about researchers producing new treatments to help people. I just think that these treatments should be supported extremely by many studies.
This is truly exciting!
ReplyDeleteAs a universal care worker, specializing in patients suffering with dementia, I see the personal effects this disease has on an individual. The fact that within 40 years it is estimated that 115 million new cases of Alzheimer’s will occur is heart breaking. With recent discoveries regarding the amyloid deposition, and its effects on the integrated neuronal cortical areas, Alzheimer’s can be classified as not only a degenerative disease, but also a multi-level breakdown along a broader system. Putting a name to a face now allows different methods of treatments to become possibilities in the fight against this debilitating disease.
Previous treatments of Alzheimer’s included Cholinesterase inhibitors and Memantine. These two types of AD medication allowed for cell connections to be increased in the hopes of slowing down the buildup of plaque causing the loss of memory recollection. Sadly, these medications only slow down the effects of the disease. There is no cure as of yet.
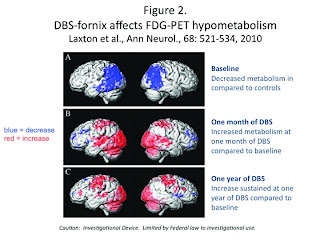
With the recent breakthroughs in AD research, circuitry-based treatment via deep brain stimulation can become a possible treatment option. Stimulating the brains hippocampal fornix can increase the neural circulation of the brain and its networks, benefitting the overall mental wellness of an AD patient.
The issue regarding DBS is the invasive procedure itself. DBS involves a neurosurgeon surgically implanting indwelling electrodes into the brain’s circuit networks. Though the initial risks are said to be low, one would have to ask if the invasive procedure would be worth it. Retarding the disease may be beneficial, yes, but at what cost? The risks towards slowing down a degenerative disease could bring immediate risks to the patient. Stroke or death could result from this neurosurgical procedure.
Alzheimer’s is a disease that in years past has been diagnosed definitively, post-mortem. Even with the possibility of DBS as treatment, the effects would only shorten the indefinite. There is no rewind for those diagnosed with the disease. I have seen the wear and tear of Alzheimer’s on patients I have learned to truly care for. I have seen the effects of current medications used. I have lost some that I truly care for. Though there may not be an end to the disease as of yet, the new research takes one step in the right direction in finding a cure.